Spondylolisthesis is a condition characterized by the partial or complete anterior displacement (slippage) of a superior vertebra relative to the inferior vertebra, resulting from an abnormality in the bony connection between adjacent vertebral bodies. This abnormality can be caused by congenital dysplasia, trauma, degeneration, or repetitive stress/strain. The condition manifests clinically with symptoms including lumbosacral pain, sciatica (involvement of the sciatic nerve), and intermittent claudication. The prevalence of spondylolisthesis ranges from 4.7% to 5%. It most commonly occurs at the L4/L5 or 5/S1 vertebral levels. | 
|
Classification and Grading of Lumbar Spondylolisthesis
Lumbar spondylolisthesis can be classified into the following types: dysplastic spondylolisthesis, isthmic spondylolisthesis, degenerative spondylolisthesis, traumatic spondylolisthesis, pathologic spondylolisthesis, and iatrogenic spondylolisthesis. Among these, the isthmic type accounts for approximately 15% of cases, while the degenerative type comprises about 35%.
1. Dysplastic Spondylolisthesis: Characterized by congenital hypoplasia of the pars interarticularis, resulting in inadequate structural support for the weight of the upper body. Often associated with spina bifida at L5-S1.
2. Isthmic Spondylolisthesis: Anterior slippage of the vertebral body occurs with essentially intact posterior structures, caused by pathology of the pars interarticularis. Divided into two subtypes:
a. Spondylolysis: A fatigue fracture of the pars interarticularis.
b. Elongated Pars: The pars is elongated without discontinuity, maintaining structural continuity.
3. Degenerative Spondylolisthesis: Caused by intervertebral disc degeneration. Predominantly occurs in middle-aged and elderly individuals.
4. Traumatic Spondylolisthesis: Results from severe acute injury to the bony hook region (pars/isthmus area), typically accompanied by pedicle fracture.
5. Pathologic Spondylolisthesis: Secondary to systemic diseases (e.g., metabolic bone disease, infection, tumor) that cause fracture or elongation of the articular facets.
6. Iatrogenic Spondylolisthesis: Most commonly occurs post-surgically due to extensive laminectomy and facet joint resection for decompression.
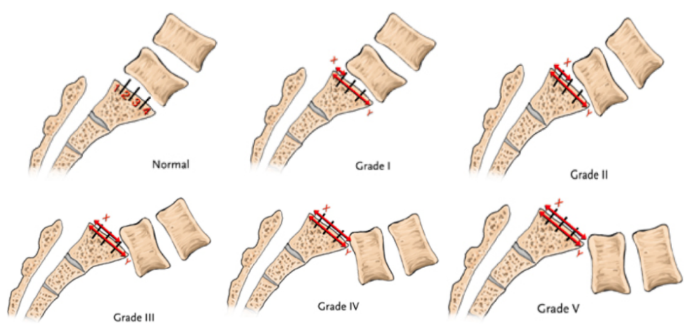
Grading of Lumbar Spondylolisthesis
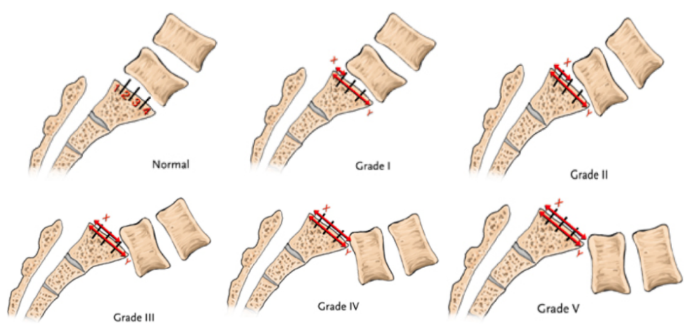 | The Meyerding classification, commonly used domestically (in China), is the standard grading system. It divides the superior endplate of the caudal (lower) vertebral body into four equal parts. The grade (I-IV) is determined by the degree of anterior slippage of the cephalad (upper) vertebral body relative to the caudal vertebral body: (Note: The original text ends here describing the Meyerding principle. The actual grades would be:) · Grade I: 0-25% slippage · Grade II: 26-50% slippage · Grade III: 51-75% slippage · Grade IV: 76-100% slippage (Grade V, spondyloptosis, >100% slippage, is sometimes included but not mentioned in the original text). |
Treatment Options for Lumbar Spondylolisthesis
For spondylolisthesis below Grade I, conservative treatment can be adopted. Patients who do not respond to conservative treatment or have higher-grade slippage may opt for surgical intervention. To minimize intraoperative bleeding, accelerate postoperative recovery, and reduce complications such as postoperative low back pain and weakness, percutaneous pedicle screw fixation is generally chosen for Grade I and II lumbar spondylolisthesis, while open reduction and internal fixation is selected for moderate to severe cases.
Conservative Treatment:
For spondylolisthesis below Grade I, conservative management includes:
· Bed rest
· Lumbar and back muscle exercises
· Wearing a lumbar brace or orthosis
· Appropriate aerobic exercise for weight reduction
· Avoiding activities that increase lumbar load (e.g., lifting heavy objects, bending forward)
· Physical therapy modalities such as infrared therapy and thermotherapy
· Symptomatic pharmacotherapy (e.g., oral NSAIDs like celecoxib or ibuprofen) for pain relief.
Surgical Treatment:
Nerve Decompression:
The primary goal is adequate nerve root decompression. This can be achieved via unilateral or bilateral laminotomy/laminectomy. If laminectomy is unavoidable, spinal fusion must be added. If symptoms are caused solely by lumbar instability without spinal stenosis, only lumbar fusion and fixation are required, and spinal canal decompression is unnecessary.
Reduction, Fusion, and Internal Fixation:
Long-term stability relies on solid biological fusion. Spinal fusion methods vary:
· Based on graft location: Interbody fusion, posterolateral fusion, 360-degree circumferential fusion.
· Based on surgical approach: Interbody fusion can be further classified as anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), or transforaminal lumbar interbody fusion (TLIF).
Direct Pars Repair:
This involves reconstruction or direct repair of the pars interarticularis. Techniques include screw fixation and hook fixation. It is suitable for young patients.
Advantages of Minimally Invasive Surgery (MIS) for Spondylolisthesis:
1. For Grade I and II spondylolisthesis, percutaneous fixation and fusion provides sufficient therapeutic efficacy.
2. Compared to the traditional posterior midline approach, MIS reduces crush injury to retracted muscles, avoids detachment of posterior ligamentous structures, and preserves the integrity of the lumbodorsal fascia. This significantly lowers the incidence of complications like postoperative low back pain and weakness.
3. MIS results in significantly less blood loss and shorter hospital stays compared to the traditional posterior midline approach.
Posterior Minimally Invasive Thoracolumbar Screw-Rod System
 | The Posterior Thoracolumbar Minimally Invasive Screw-Rod System strictly adheres to MIS (Minimally Invasive Surgery) principles in its product and instrument design, ensuring safety, reliability, and user-friendly operation. Safe and Reliable Product Design: · Dual-threaded design enhances screw pullout strength by 13-20%. 
|
Triple-Core Design: · Tail Tapering Design: Continuously enhances the compression effect on the pedicle cortical bone, strengthening pullout resistance. · Tip Flute Design: Facilitates screw guidance and insertion. 
| Screw plug with negative-angle thread design; prevents thread stripping caused by tail expansion. Screw plug with pre-locking protrusion design; enhances gripping force on the titanium rod. 
|
Tool Design Features
1. Nail insertion and rod placement are simple and reliable.  
| 2. Multiple Reduction Options  Method I: Reduction via Sliding Reduction Plate Method I: Reduction via Sliding Reduction Plate | 2. Multiple Reduction Options  Method II:Reduction using Rod Pusher |
3. Multiple Distraction/Compression Modes  
|
Brief Description of Surgical Steps
1.Fluoroscopic localization to confirm the surgical level(s) and the skin incision site. 
| 2.Incise the skin 
| 3.Initial trocar placement and positioning 
| 4.Insert guidewire |
5.Place dilating tubes 
| 6.Breach cortical bone and tap the pedicle tract 
| 7.Insert pedicle screw 
|
8.Reduce the spondylolisthetic 
| 9.Establish minimally invasive access for cage/implant insertion 
| 10.Prepare the intervertebral disc space
 

|
11.Insert interbody cage 
| 12. Confirm appropriate cage  
| 13.Pass the rod 
|
14. Place set screws (onto screw heads)

| 15. Apply compression 
| 16. Torque set screws to final lock  | 17.Remove rod inserter

|
18. Disengage screw extenders 
| 19. Suture skin  |