Osteoporosis is a clinically significant and prevalent geriatric disease today, often presenting with comorbidities such as diabetes and other chronic conditions.
01 Definition of Osteoporosis

Osteoporosis is a metabolic bone disease characterized by decreased bone mass and deterioration of bone tissue microstructure, leading to increased bone fragility and susceptibility to fractures. Clinically common, osteoporosis is often associated with osteoarthritis and fundamentally represents a disorder of bone metabolism. The primary cause is insufficient osteoblast activity, resulting in reduced bone formation, coupled with enhanced osteoclast activity, leading to increased bone resorption. Another contributing factor is inadequate nutrition in early life, which lowers peak bone mass and predisposes individuals to fractures in later years.
02 Hazards of Osteoporosis
· Pain: Primarily manifests as low back pain, though systemic skeletal pain may also occur; pain worsens with physical exertion; difficulty turning over, changing positions, and walking.
· Fractures: Minor bumps or even coughing may lead to fractures. Common sites include the spine, hip, proximal humerus, and distal forearm.
· Spinal deformities, kyphosis (hunchback), limited extension, and height loss.

03 How to Know if You Have Osteoporosis
· Fragility Fracture: The occurrence of a fragility fracture is sufficient for a clinical diagnosis of osteoporosis.
· Low Bone Density: Bone mineral density (BMD) measurement is performed.
· Exclusion of Other Diseases Affecting Bone Metabolism: Other diseases that impact bone metabolism must be ruled out.
The measurement obtained by Dual-Energy X-ray Absorptiometry (DXA) is currently the globally recognized gold standard for diagnosing osteoporosis. The T-score = (Measured Value - Peak Bone Mass of Ethnicity-matched Healthy Young Adults of the Same Sex) / Standard Deviation of Bone Mineral Density in Healthy Young Adults.

04 Pharmacotherapy for Osteoporosis
· Bisphosphonates: These are synthetic, non-biodegradable pyrophosphate analogs. They inhibit osteoclast-mediated bone resorption, effectively increase bone mineral density (BMD), and possess the fundamental actions of inhibiting both bone resorption and calcification. This leads to a reduction in fracture risk for patients with postmenopausal osteoporosis and osteoporosis due to other causes.
· Calcitonin: Calcitonin is a hormone secreted by thyroid C cells that inhibits osteoclast activity. It specifically and directly binds to receptors on osteoclasts, reducing their activity and number, slowing their maturation process, and thereby inhibiting bone resorption.
· Parathyroid Hormone (PTH): Parathyroid hormone is the primary hormone regulating calcium and phosphorus metabolism and maintaining systemic calcium balance. It increases the number of osteoblasts and stimulates them to release bone growth factors, thereby promoting bone formation. Concurrently, it can extend the lifespan of osteoblasts by inhibiting apoptosis.
· Estrogen: Estrogen is a critical factor in maintaining the balance between bone resorption and formation. It has long been regarded as the standard protective agent for postmenopausal women.
· Other Medications: Drugs such as Strontium Ranelate and Vitamin K also demonstrate certain efficacy in treating osteoporosis.
Of course, treating osteoporosis cannot rely solely on medication. Daily Precautions and Dietary Care are also particularly crucial.
05 Treatment of Fractures in Patients with Osteoporosis & Introduction of Atom Medical Products
Currently, the primary clinical treatment for traumatic fractures is surgical internal fixation. Locking Plates and Intramedullary Nails are the most widely used internal implants in clinical practice, offering superior biomechanical performance compared to other implants.
However, in recent years, a significant and increasing number of fracture patients also present with osteoporosis. In these patients, the bone provides poor implant anchorage, making implant cut-out and migration relatively common postoperative complications.
To address this issue, Atom Medical has developed the Balloon Bone Cement Internal Fixation System. This system innovatively integrates balloon expansion and bone cement filling into traumatic internal fixation surgery, significantly enhancing the strength of the fixation. It achieves stable internal fixation even in cases of osteoporotic fractures. This system comprises two main types:
· Balloon Bone Cement Locking Plate System
· Balloon Bone Cement Intramedullary Nail System
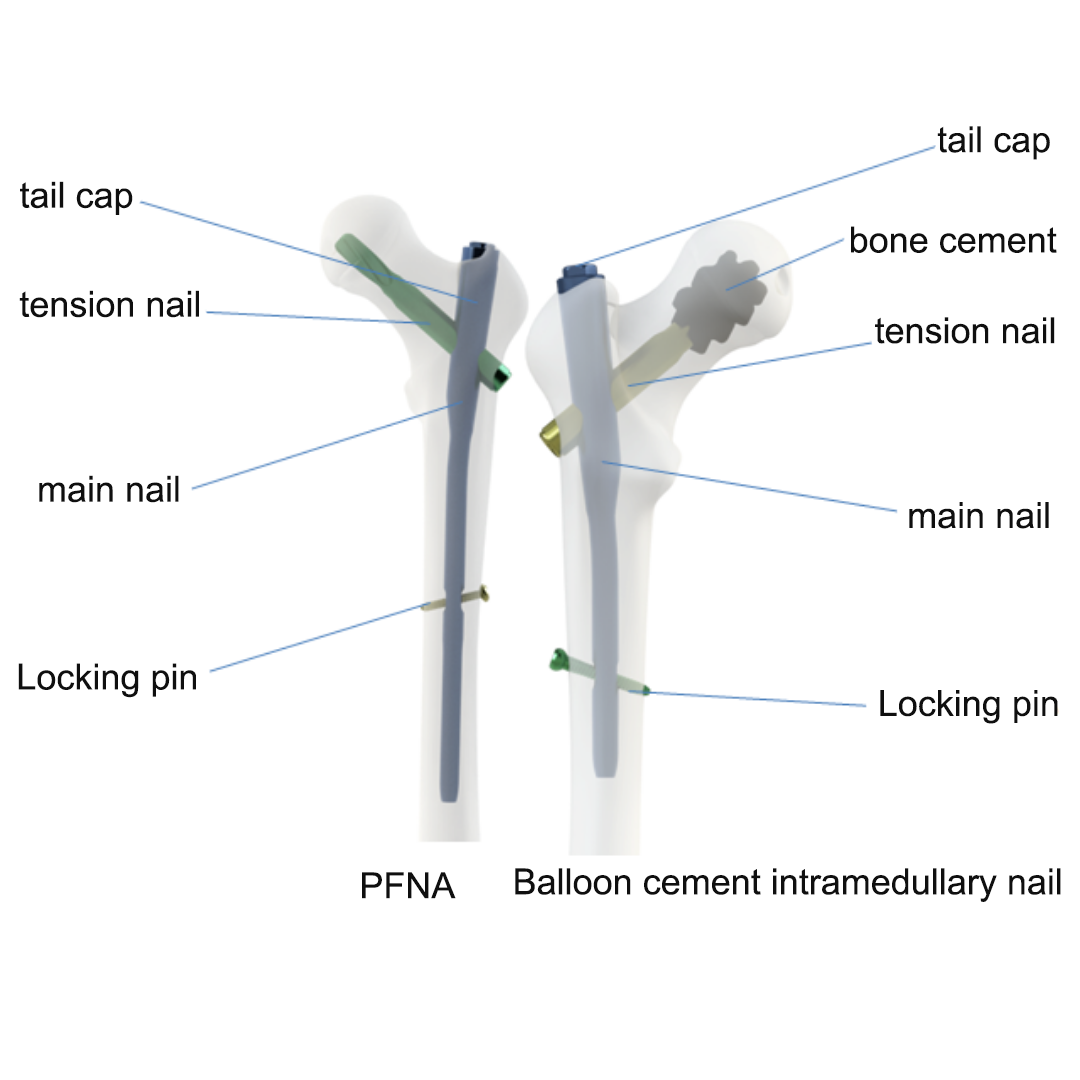
Taking the Balloon Cement-Augmented Intramedullary Nail System as an example, we can compare it with the commonly used traditional PFNA (Proximal Femur Nail Antirotation). Traditional PFNA fixation, as shown in Figure 1, consists of an intramedullary nail (main nail), a lag screw, locking screws, and an end cap. The lag screw is typically a helical blade design.
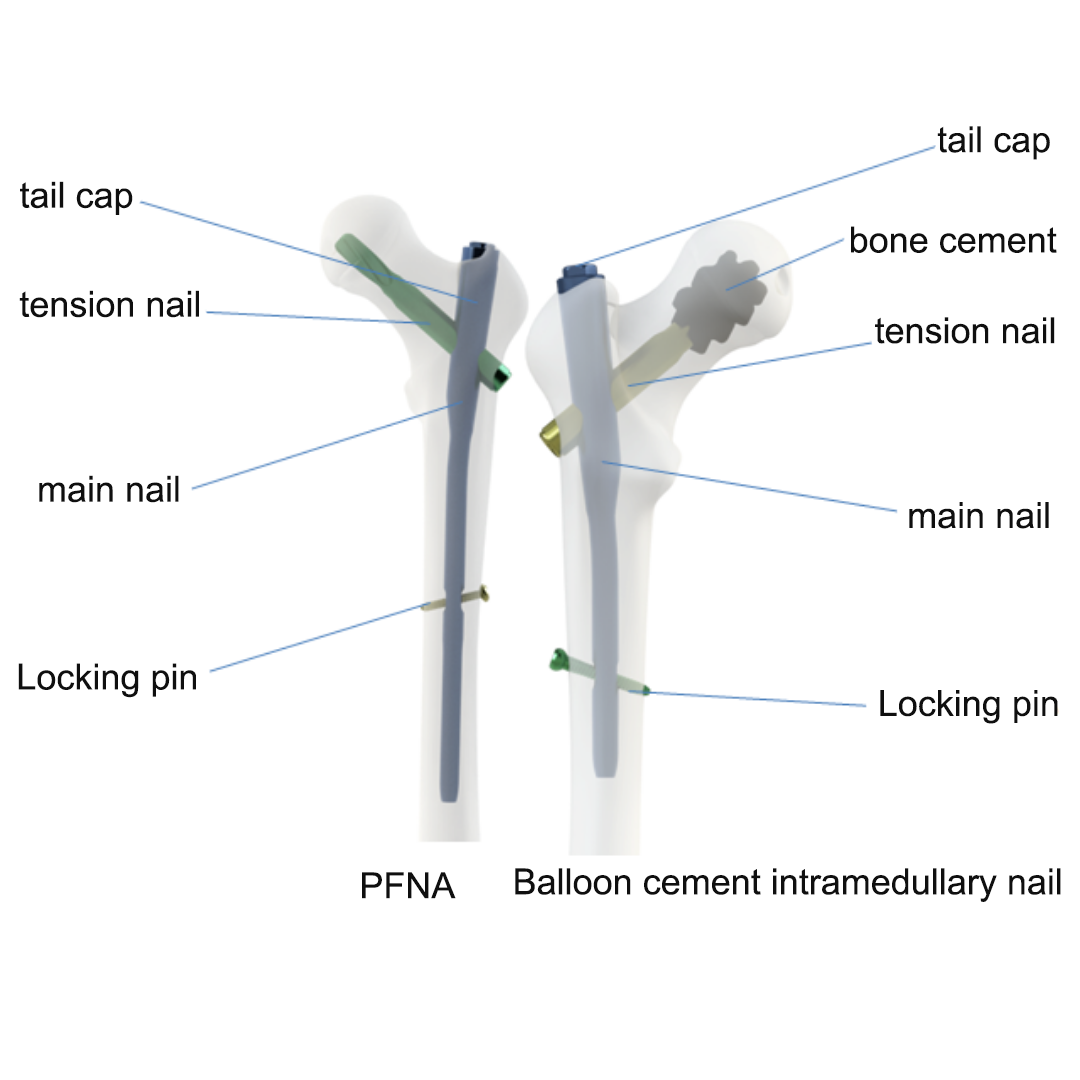 | Atom Medical's Balloon Bone Cement Intramedullary Nail System, as shown in left, consists of an intramedullary nail (main nail), a bone cement lag screw, locking screws, and an end cap. The bone cement lag screw, depicted in Figure 3, is designed with bone cement diffusion holes. These holes are utilized in conjunction with the balloon and bone cement during the implantation procedure. This system incorporates an additional step of balloon expansion and bone cement injection compared to traditional surgery. This dual-action approach simultaneously compresses the intra-articular bone environment and creates a cavity for bone cement filling. |
 |
As shown in Figures 4-5, the procedure is performed as follows: First, a cavity is expanded within the joint space using balloon dilation instruments. Subsequently, the prepared bone cement is injected through the central cannulation of the helical blade into the distal end of the pre-drilled screw tract within the femoral head using an injection device. Following cement injection, the helical blade is advanced into the original tract. Finally, fluoroscopy is employed to verify the final position of the helical blade and the distribution pattern of the bone cement.
To validate the effectiveness of the traditional Proximal Femoral Nail Antirotation (PFNA) system and the balloon bone cement intramedullary nailing system, 54 elderly patients with intertrochanteric femoral fractures were selected as the study subjects. All patients sustained their injuries from ground-level falls. Fractures were assessed using the Evans-Jensen classification; the degree of osteoporosis was evaluated using the Cortical Thickness Index (CTI) of the affected femur. Inclusion criteria were: (1) A clear history of trauma; (2) Age ≥ 75 years, with CTI of the affected femur < 0.4; (3) Confirmed diagnosis of Evans-Jensen type I-V intertrochanteric femoral fracture via imaging (X-ray or CT) examination, requiring surgical intervention.
All 54 patients successfully underwent surgery. At the final follow-up, no cases of internal fixation failure were observed in the balloon bone cement nail group. In the traditional PFNA group, 2 cases (8.3%) of internal fixation failure occurred: one case of cut-out and one case of implant fracture. The average displacement was 0 mm in the bone cement group and (1.4 ± 3.39) mm in the traditional PFNA group. The final Functional Recovery Scores (FRS) at the last follow-up were 81.17 points for the bone cement group and 76.43 points for the traditional PFNA group. These results indicate that the balloon bone cement internal fixation system can enhance the stability of the lag screw, preventing screw loosening and cut-out, thereby improving the fixation effectiveness of the implant.
In conclusion, Atom Medical's balloon bone cement internal fixation system effectively addresses the challenge of internal fixation for osteoporotic fractures. It provides high fixation strength and rarely exhibits complications such as implant displacement or cut-out, which are relatively common with traditional products.
06 // Postoperative X-ray
 |  |
Atom Medical PFNA with Bone Cement Postoperative AP View | Atom Medical PFNA with Bone Cement Postoperative Lateral View |